Public Law 99-158, the Health Research Extension Act of 1985, creates the National Center for Nursing Research (NCNR) at NIH.

Dr. Dorris Merritt, Special Assistant to the NIH Director, is appointed Acting Director of the National Center for Nursing Research (NCNR). NCNR's initial budget is $16 million.

The NCNR Advisory Council holds its inaugural meeting. The council (now known as the National Advisory Council for Nursing Research) provides recommendations on the direction and support of the nursing, biomedical, social, and behavioral research that forms the evidence base for nursing practice.

Dr. Ada Sue Hinshaw serves as the first Director of the National Center for Nursing Research (NCNR).

Dr. David Olds and colleagues establish that visits from home nurses significantly lower mothers' high blood pressure during pregnancy, result in better timing of subsequent pregnancies, and reduce abuse and neglect of children.

The National Center for Nursing Research (NCNR) is elevated to an NIH Institute, becoming the National Institute of Nursing Research (NINR), after the NIH Revitalization Act of 1993 is signed into law.

DHHS Secretary Donna Shalala signs the Federal Register notice establishing the National Institute of Nursing Research (NINR).

Dr. Loretta Sweet Jemmott tests several gender-appropriate, culturally sensitive interventions on hard-to-reach vulnerable populations and significantly reduces sexual risk behaviors for HIV.
Her "Be Proud! Be Responsible!" intervention becomes the Centers for Disease Control and Prevention's model curriculum.

Dr. Suzanne Hurd serves as Acting Director of NINR.

Dr. Patricia A. Grady is appointed Director of NINR.

The NIH Director designates NINR as the lead NIH Institute to coordinate collaborative research at NIH and other Federal Agencies on end-of-life care.
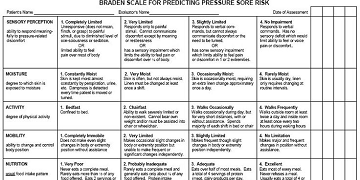
Dr. Nancy Bergstrom, in a multi-site study, tests the Braden scale for risk of pressure sores and finds its predictive capability accurate. The scale is widely used in nursing homes and hospitals. Image courtesy of Dr. Nancy Bergstrom.

Dr. Joanne Harrell, building on research that showed risk for cardiovascular disease can begin at an early age, demonstrates that a specially designed classroom educational program for elementary school children could significantly lower their cholesterol levels in just eight weeks.
Dr. Mary Naylor demonstrates that transitional care from hospital to home can significantly improve the health of older adult patients and substantially reduce patient days in hospitals, hospital readmissions, and health care costs.

Dr. Jon Levine establishes that gender plays a key role in pain relief, with women obtaining satisfactory relief from kappa-opioids while men receive little benefit.

Dr. Margaret Grey reports that providing training in coping skills–such as social problem solving, communication, and conflict management–for young people with type 1 diabetes mellitus can significantly improve their quality of life.

NINR holds the first Summer Genetics Institute (SGI), a two-month, full-time summer research training program targeted at faculty, graduate students and advanced practice nurses.
NINR launches a free online training, "Developing Nurse Scientists" for students interested in the nursing research field.

Dr. Linda Aiken demonstrates that hospital working conditions and adequacy of nurse staffing per patient can affect patients' recovery. In hospitals where nurses have lower patient workloads, patients have substantially lower mortality rates.
In later work, Dr. Aiken and collaborators discover that increases in the numbers of nurses on staff with bachelor's degrees lowers the likelihood of patient death.
Dr. Martha Hill finds that interventions conducted at the community level by a multidisciplinary health care team reduce high blood pressure in young inner-city African-American males, who are typically underserved by the health care system. The study illustrates that culturally sensitive, successful interventions can be conducted for vulnerable populations and can help reduce health care disparities.
NINR launches a new pilot training project, the Graduate Partnerships Program in Biobehavioral Research.
NINR commemorates its 20th anniversary at NIH and plays an integral role in the NIH Roadmap Initiative, which was launched by the NIH Director to address opportunities and gaps in research that will accelerate the progress of science.
Dr. Bernadette Melnyk demonstrates that her Creating Opportunities for Parent Empowerment (COPE) program, which aims to support the parents of premature infants, results in improved knowledge and parenting behaviors, decreased parental stress, and shorter length of NICU stays, reducing health care costs associated with premature births by about $4,800 per infant. COPE has since been adopted by hospitals and insurers throughout the United States.
Dr. J. Randall Curtis and collaborators report that an intervention to improve communication between ICU clinicians and family members of dying patients significantly reduces feelings of stress, anxiety, depression, and other symptoms of post-traumatic stress disorder in the family members for up to three months after the loss of their loved one.
Dr. Pamela Mitchell reports that a behavioral intervention called Living Well with Stroke reduces the incidence of depression in stroke survivors, both immediately after treatment for stroke and at a one-year follow up.

NINR publishes an award-winning patient information brochure, “Palliative Care: The Relief You Need When You're Experiencing the Symptoms of Serious Illness,” which is available in English or Spanish.

Dr. Wendy Henderson, an NINR intramural researcher, develops a device for collecting patient-reported outcomes related to pain called the "Gastrointestinal Pain Pointer", enabling a patient to describe the location, intensity, and subjective components of their pain on a graphic interface.

NINR commemorates its 25th anniversary at NIH with a series of scientific events.
NINR intramural researcher Dr. Taura Barr identifies a gene panel useful for stroke diagnostics and outcome prediction as well as other neurological conditions such as traumatic brain injury.
The Palliative Care Research Cooperative Group (PCRC) is established with foundational support from NINR to develop scientifically based methods that lead to meaningful evidence for improving quality of life for patients with advanced or potentially life-limiting illnesses, and their caregivers — including family members and providers of care. The network creates a community of palliative care providers who can engage in research discovery.
The research of Drs. Rita Colwell, Anwar Huq, and colleagues shows that using readily available sari cloth to filter pond and river water successfully reduced the incidence of cholera by nearly half in a study conducted in Bangladesh.

NINR holds the first Methodologies Boot Camp for nursing graduate students, faculty and clinicians, which focuses on pain research.
NINR releases its history book, NINR: Bringing Science to Life, in commemoration of the Institute's 25 years at NIH.

NINR establishes a YouTube channel, “NINR News,” to post videos highlighting its events, trainings, and initiatives.

NINR launches a new NINR Director's Lecture series, designed to bring the nation's top nurse scientists to the NIH campus to share their work and interests with a transdisciplinary audience.
Dr. Bernadette Melnyk presented the inaugural lecture on “COPE: Improving Outcomes for Premature Infants and Parents.”

Dr. Barbara J. Drew leads a team that develops a modified electrocardiogram technique that can quickly be administered by a paramedic with the results automatically transmitted to the hospital via cell phone.
This allows hospital personnel additional time to prepare for the incoming patient, potentially leading to faster treatment and improved patient outcomes.
As part of its 25th Anniversary Commemoration, NINR presents a workshop on "Introduction to Research Grantsmanship for Early Career Nurse Scientists" at regional nursing research conferences across the country. The workshop highlights NINR's mission of training the next generation of biomedical and biobehavioral nurse scientists. It is appropriate for pre- and post-doctoral students and early career nurse scientists. The workshop is then developed into video presentations located on NINR's website and YouTube channel.
Dr. Samuel Sia and colleagues develop a novel “lab-on-a-chip” device for rapidly detecting HIV. This lab-on-a-chip, or mCHIP can quickly, accurately, and cost-effectively detect clinically infectious diseases in resource-limited settings.

NINR organizes a national summit on “The Science of Compassion: Future Directions in End-of-Life and Palliative Care,” attended by nearly 1,000 scientists, health care professionals, and public advocates.
NINR releases its new Strategic Plan, Bringing Science to Life, which outlines the role NINR-supported science can play in addressing the nation's most pressing healthcare challenges, and details NINR's strategic priorities for scientific research over the next five years and beyond.

Dr. David Dinges and collaborators study individuals with an alteration in a protein called catechol-O-methyltransferase (COMT), and find that this mutation could serve as a biomarker to predict individual differences in sleep physiology and further our understanding of the effects of sleep deprivation.
Dr. Marilyn Rantz finds that, in a trial of an early warning sensor system that alerts nurses to declining health, long-term care residents participating in the intervention demonstrate better functional measures (e.g., hand-grip; gait) than residents receiving usual care. Later Dr. Rantz and collaborators conduct research on the development of a sensor system for use in apartments in a senior living community. The sensors alert nurse-care coordinators and clinicians to alterations in a patient’s health before the appearance of clinical signs–knowledge that can help promote independent living for older adults.

NINR publishes “Building Momentum: The Science of End-of-Life and Palliative Care: A Review of Research Trends and Findings, 1997–2010.” This report looks at the trends in end-of-life and palliative care (EOL PC) research publications over the past 14 years.
NINR launches its Innovative Questions (IQ) Initiative, the next step in the implementation of NINR's Strategic Plan.

The Office of End of Life and Palliative Care Research is established to support NINR's leadership role in end-of-life and palliative care research.
Dr. Jessica Gill, one of the first Lasker Clinical Research Scholars and an NINR intramural investigator, and Dr. Ida Spruill, an NINR-supported extramural scientist, are selected to receive the Presidential Early Career Award for Scientists and Engineers (PECASE), the highest honor bestowed by the United States Government on science and engineering professionals in the early stages of their independent research careers.

NINR launches the Palliative Care: Conversations Matter® campaign, which aims to increase awareness of and improve communications around pediatric palliative care. The campaign has resources in English and Spanish for providers and families.
NINR develops a new web resource aimed at helping people address a sensitive subject – the end of life. The 13-chapter End of Life module was added to NIHSeniorHealth.gov, a health and wellness website for older adults.

NINR releases the video “Nursing Research: Bringing Science to Life.” In the video, NINR Director Dr. Patricia A. Grady gives an overview of NINR and discusses the role that nursing research plays in advancing health.

Dr. Hyekyun Rhee and an interdisciplinary team of researchers develop and test an automated device for asthma monitoring (ADAM), applying technology to help assess asthma symptoms objectively and accurately. Image courtesy of Dr. Hyekyun Rhee.
The device is found to be a valid asthma monitoring tool, and was well-received by users. These results indicate that ADAM can improve self-management of asthma in adolescents.

NINR hosts a briefing on the IOM report, Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life.

Dr. Amy Abernethy and others in the NINR-supported Palliative Care Research Cooperative Group find no significant differences in mortality between patients with advanced, life-limiting illness who had discontinued statin therapy and those who had not.
NINR intramural researcher Dr. Jessica Gill leads a team which discovers that a protein linked to short-term complications after traumatic brain injury (TBI), may also be responsible for long-term complications that can result from TBI.

NINR marks its 30th anniversary at NIH with a series of scientific events and activities including the “Advancing Science, Improving Lives” scientific symposium.

NINR releases a series of videos that give an overview of opportunities and dilemmas often encountered by midcareer scientists as they work to develop a sponsored project into a successful and sustained program of research.

NINR holds its first Science and the Public Lecture. Ellen Goodman presents her talk, which describes The Conversation Project, a public health campaign and movement, that works to change the way people talk about, and prepare for their end-of-life care.

NINR releases its new Strategic Plan, Advancing Science, Improving Lives: A Vision for Nursing Science. The blueprint for the Plan grew from the Institute's 2011 Strategic Plan, past scientific accomplishments, and current research priorities.

NINR creates a LinkedIn page to provide information on NINR events, job openings, and funding and training opportunities.
NINR launches a “Stories of Discovery” web feature that highlights nursing science. The Stories of Discovery webpage puts a spotlight on programs of research from NINR-funded institutions around the country. The discoveries cross the spectrum of strategic priority areas including self-management, symptom science, and end-of-life care.
NINR intramural researcher Dr. Jessica Gill and colleagues find that the blood protein tau can be an important new clinical biomarker to better identify athletes who need more recovery time before safely returning to play after a sports-related concussion.
Dr. Jacquelyn Taylor, an NINR-supported investigator at Yale University, was among those named as recipients of this year's Presidential Early Career Award for Scientists and Engineers (PECASE).
An early integrated palliative and oncology care intervention developed by Dr. Jennifer S. Temel and colleagues finds that patients receiving the intervention are more likely to have discussed their preferences in end-of-life care with clinicians and to report that knowing their prognoses was helpful in decision-making. The study's findings indicate a significant positive impact of discussions with palliative care clinicians on patients with incurable cancer.

The NINR Intramural Research Program holds a scientific symposium, “Symptom Science Research: A Path to Precision Health,” highlighting Intramural's scientific advances and collaborations across the NIH and other organizations.
NINR and its partners host “The Science of Caregiving: Bringing Voices Together” Summit. The Summit provides perspectives across the spectrum of caregiving, including the importance of caregiving across the lifespan as well as current and future directions for research to improve the health of patients and caregivers.
NINR implements a new email subscription service to make it easier to learn more about NINR topics. In addition to the News and Notes newsletter, NINR is now offering subscription topics related to events, training, and palliative care.
Research led by Dr. Paul Macey, discovers connections between obstructive sleep apnea (OSA) symptoms and thinning of the brain's cerebral cortex. The study also discovers differences in these brain changes among men and women, which might explain why women are more likely than men to have cognitive symptoms like depression, insomnia, and anxiety when experiencing OSA.

After 23 years of service, Dr. Patricia A. Grady retires as director of NINR.

Dr. Ann Cashion serves as Acting Director of NINR. On September 30, 2019, Dr. Cashion retires from federal service.
NINR teams up with the National Library of Medicine’s MedlinePlus to launch a text message campaign for those living with serious illnesses and their families. The campaign offers weekly text messages about palliative care in English and Spanish.
NINR hosts the “Precision Health: Smart Technologies, Smart Health” Symposium. The symposium features scientific panels and a poster session aimed at engaging graduate nursing students, nursing faculty, and clinicians interested in the clinical applications and clinical focus of smart health, smart technologies, digital health data, wearables and sensors, virtual/augmented reality, and molecular omics data.

To advance the growing importance of “omics” in nursing science, NINR develops the Omics Nursing Science & Education Network (ONSEN) website in collaboration with the National Cancer Institute (NCI) and the National Human Genome Research Institute (NHGRI).

Dr. Michal A. Elovitz and colleagues compare the cervicovaginal microbiota of women with spontaneous preterm births versus women delivering at term to better understand if the microbial environment is a factor. Read the abstract on PubMed. Read the full open access article at Nature Communications.

Dr. Paule V. Joseph is selected as a Lasker Clinical Research Scholar within the NINR Division of Intramural Research, with a joint appointment with the National Institute on Alcohol Abuse and Alcoholism (NIAAA). Dr. Joseph has also been a member of the NIH Distinguished Scholars Program since 2018.
NINR's Division of Intramural Research hosts a scientific symposium to mark the launch of the NINR-led Symptom Science Center, a trans-NIH resource for the scientific community.
NINR-supported investigators, Drs. Sarah (Collins) Rossetti, and Tracey L. Yap, receive the Presidential Early Career Award for Scientists and Engineers (PECASE).
Dr. Lawrence Tabak serves as Acting Director of NINR.
Dr. Tara A. Schwetz serves as Acting Director of NINR.

Shannon N. Zenk, PhD, MPH, RN, FAAN, joins NIH as the director of the National Institute of Nursing Research.